Dr. Daniel Micallef
Friday, 17 May 2024
15:00 – 15:20 CEST
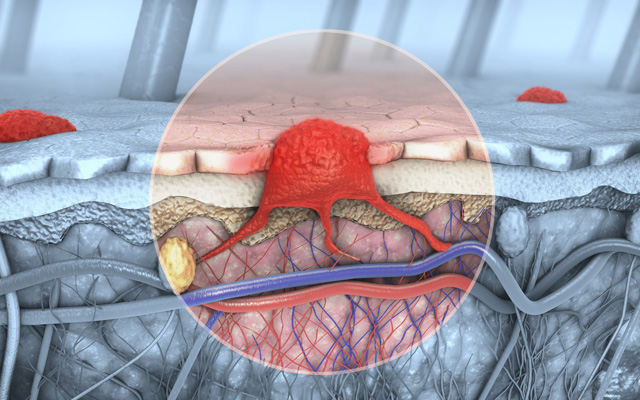
Cutaneous melanoma can potentially metastasise to lymph nodes, skin, and subcutaneous tissue as well as internal organs such as the lungs, liver, bone and brain. Melanoma responds poorly to cytotoxic chemotherapeutic agents and the gold standard treatment since the 1970s had been single-agent dacarbazine which only achieved an overall survival of 7.4 months. Later on, in the 20th century, more durable responses were obtained with interleukins such as interleukin-2. However, the overall response rate was still around 15%.
It was the advent of immunotherapy and targeted therapy which revolutionised the management of advanced melanoma. CTLA-4 inhibitors such as ipilimumab were the first immunotherapeutic agents used in this setting. These molecules prevent B7 ligands from binding to CTLA-4 on T-cells, resulting in increased T-cell activation and immune recognition of tumour cells. Since then, several other immunotherapeutic agents have been developed. PD-1 inhibitors such as nivolumab prevent the binding of PD-L1 to PD-1 on T-cells, restoring the immune recognition and destruction of tumour cells. Immunotherapy can offer lasting responses in a significant proportion of patients but comes with risks of serious adverse effects which can be permanent. More recently, LAG-3 inhibitors (relatlimab) have been developed and approved for use in advanced melanoma. LAG-3 inhibition allows T-cell responses to remain active against tumour cells. They are associated with less systemic toxicity when compared to CTLA-4 blockers.
Apart from immunotherapy, targeted therapy has been used in the management of advanced melanoma. Activation of the MAP kinase pathway is important in melanoma oncogenesis. The commonest mutations, present in around 50% of cutaneous melanoma are in codon 600 of the BRAF oncogene. BRAF V600E and V600K mutations would be amenable to treatment by BRAF inhibitors such as dabrafenib or encorafenib which generally show dramatic response rates, but resistance develops within an average of 6 months. The addition of a MEK-inhibitor such as trametinib or binimetinib can delay the onset of resistance extending the median progression-free survival to around 11 months. MEK-inhibition may also play a role in NRAS mutant melanomas.
Developments in immunomodulatory and targeted therapies have dramatically transformed the treatment landscape for advanced melanoma. While more research and studies are ongoing, their treatment options, sometimes combined with more traditional modalities, lead to improved patient outcomes in previously considered untreatable situations.